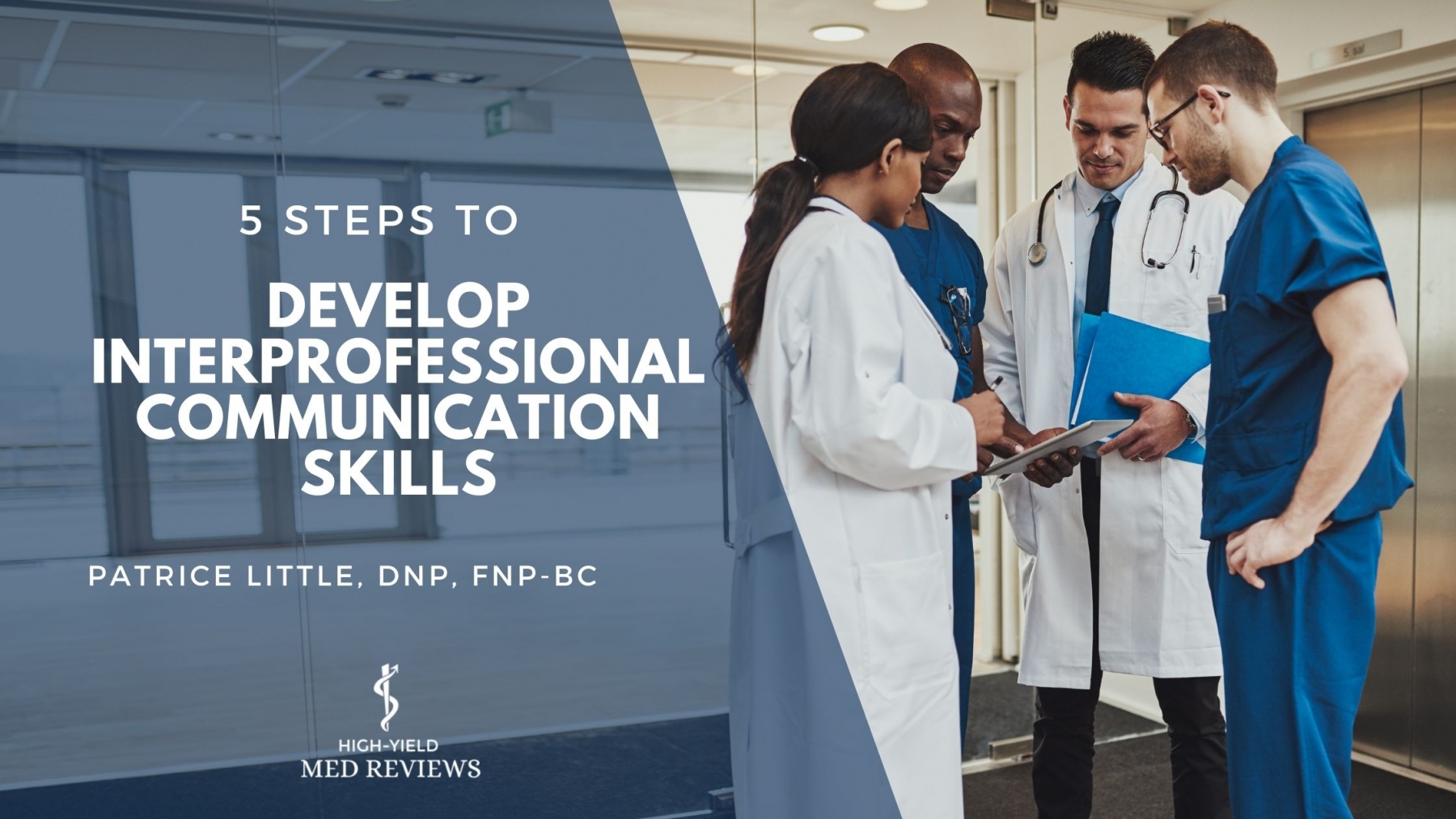
5 Steps to Develop Your Interprofessional Communication Skills
By Patrice Little, DNP, FNP-BC
"The single biggest problem in communication is the illusion that it has taken place"
George Bernard Shaw
When I think of
efficiency, Starbucks comes to mind. Each time I receive my steamy, tall mocha
latte with almond milk and no whip I am confident that it will be just that.
Now, that is just one drink combination out of thousands, yet as a
consumer, I expect them to get it right whether it is a Starbucks in Dallas or
Atlanta. They have a system that incorporates ongoing communication,
collaboration, documentation, and evaluation among the team. This ultimately
makes Starbucks known for its best practice in the making and presenting of
coffee drinks.

Similarly, the healthcare
system has many moving parts. Interprofessional collaboration (IPC), the teamwork
of two or more health professionals from different disciplines, is commonly
known as a proactive approach to ensuring efficient use of the healthcare
system by patients. The World Health Organization (WHO) affirms that IPC
encourages communication, reduces healthcare costs, promotes healthcare
innovation, and ultimately, improves patient outcomes. However, there is
little to no discussion on how to coordinate IPC in nursing, NP, or PA school when IPC skills
are an essential responsibility of these healthcare team members as leaders.
IPC encourages communication, reduces healthcare costs, promotes healthcare innovation, and ultimately, improves patient outcomes.
IPC values the
knowledge and skills of each discipline for decision-making and knowing how to
communicate both is the first step in developing IPC skills. Nurse Attorney,
Michelle Swift, noted that communication failures were a contributing factor in
27% of medical malpractice claims and effective interprofessional communication
was found to improve care, reduce medical errors, as well as injuries. Nurse
practitioners are not exempt from malpractice suits when it comes to
collaborative care. We are all familiar with the story of a patient who was
seen by both the physician and the NP who unfortunately died because of communication
gaps. The formula for communication in healthcare can be complex due to the
fragmentation of language, used to share vital information in a short amount of
time. Here are five steps for developing your interprofessional communication skills
as a leader:

1. Identify
the key players involved in the care team.
Communication
begins at the point of entry of patient care, involves multiple players, and
continues until the care is resolved. The players involved depend on factors
such as the facility, specialty, and acuity of the patient receiving the care. For
instance, the interprofessional team for primary care may involve the following
players: a collaborative or supervising physician, nurse practitioner, specialist,
pharmacist, registered nurse, medical assistant, receptionist, and the patient-family
unit. Whereas a care coordinator may be included in acute care, because patients
in this setting may require more players. Although each player is not a
licensed health professional, leaders are encouraged to get to know them and
how their knowledge and skills fit into the patient's care. After you identify the players, introduce
yourself as a resource so you can build a professional relationship with them.
Next, get to know what services they provide and how to contact them for
emergencies. This ameliorates communication barriers among the team, when
everyone is familiar with each other. Ultimately, building relationships with
the team is key to avoiding communication gaps and ensuring care is
streamlined.

2. Use
the correct communication tool.
Tools such as the electronic
medical record (EMR) and care pathway capture and guide the
team's communication, respectively. The team uses the EMR to document and track
patients' progress, prescriptions, treatments, and referrals. It also allows
for transparency and houses care pathways to coordinate care. It is important
to mention that the term "care pathway" has been used interchangeably with the term
"guidelines." Care pathways list out the health professionals and their
services to support and manage patients' care. However, the National Academy of Medicine
(NAM) says practitioners follow clinical guidelines to help them with their decision-making
to confirm a diagnosis, the right medications to treat it, and when to refer
the patient to a higher level of care provided by a specialist or emergency
services. Also, consider sharing a patient-friendly version of the care pathway
with patients to communicate who's involved in their care and the services they
receive from them.
3. Be
clear about the care.
Clear, concise,
and continuous communication is necessary for any discipline. Case in point, the
Starbucks system ensures the barista is clear on the type of drink before
it is made. Likewise, the team should be clear on the diagnosis and treatment
plan before the patient's care starts. For this reason, care pathways should be
introduced to new players to prevent pathway gaps when there is a staff change.
Scheduled meetings are also encouraged, to share updates on the patient's
progress as well as needs so that appropriate interventions can be implemented.
The frequency of meetings is not as important as the information shared to
ensure continuity of care.

4. Focus
on the patient.
Developing and
maintaining a relationship with each patient should be the focus of the team.
This includes learning about them as a person, continuously encouraging them to
be involved in their care, and supporting them with their decisions. Today's
patients may present with multiple comorbidities that require more than one
care pathway. As a result, patients can easily become overwhelmed with
navigating their conditions. The practitioner is encouraged to identify the
problem the patient wants to work on first to decrease the feelings of
overwhelm. The patient should also be allowed to ask questions about their care,
and the patient should be educated on the role of each player throughout their visit
or hospital stay.

5. Evaluate
the care.
Continuous communication
among the team is encouraged until the desired health outcome is achieved for
each patient, and the steps of the care pathway should be revisited if the
patient's status has not improved. Evaluation of care requires the frontline healthcare team members caring for the patient to respect
the recommendations of key players when the care pathway requires revision and respect
the input of the patient who is being treated. It also positions them to
identify the onset of new symptoms and begin interventions.
What would Starbucks be like if
it wasn't efficient?
The other day I
experienced a first; one Starbucks barista continually taking orders while the
other tried to keep her head above water in making the drinks. I couldn't help
but notice the frustration of customers who were waiting for their drinks. When
it was my turn, I suggested that the ladies catch up before taking my
order. After all, no one was behind me.
It appeared that these two were more focused on taking orders to clear the line
than fulfilling them. As a result, they made errors in preparing the drinks,
overlooked a few orders that were not documented correctly, and had angry
customers.
This reminded me
of my first year as an RN, when I noticed my patient winking at me while
receiving a report during shift change. I asked the nurse if she noticed any different
behaviors in the middle of the night because his eye was now twitching. She
replied, "He's here for a brain bleed so that's going to happen." However, I did not recall seeing a twitch
while caring for him the previous day. Immediately, I alerted my preceptor who
in turn contacted the neurologist. Within minutes the patient started to seize
and was transferred off the floor for further evaluation of a new bleed. At
this time there was no care pathway in place and the communication gaps almost
cost this man's life. Effective and appropriate communication is essential to close the gap in IPC and improve patient outcomes. Healthcare professionals must be leaders and invest in their own development of effective communication skills and methods of interprofessional collaboration. As each of the members of the healthcare team do this, they will elevate their professions and help move us towards the goal of improving healthcare and achieving better outcomes for patients.
Patrice Little, DNP, FNP-BC
Founder & CEO, NP Student
Hi! I'm a Family Nurse Practitioner and writer who leads a lifestyle and educational resource that helps better position Nurse Practitioner (NP) students for life, career, and business. I am candid about my wins and regrets in life. I also encourage NP students to embrace their own so they can live their best life as a provider.
Interested in learning how to
communicate like a pro? NP Student University offers communication training
on-demand.